DNA is a history book – a narrative of the journey of our species through time. A shop manual, with an incredibly detailed blueprint for building every human cell. It’s a transformative textbook of medicine, with insights. These insights give health care providers immense new powers to treat, prevent, and cure diseases.”
Genetics and Genomics
Gene study exists in 2 facets: genetics and genomics. Genetics is the study of single genes in isolation. Genomics is the study of all the genes in the genome, their interaction with each other, and with the environment. Each individual’s history book is full of possible stories. The stories tell of their influence by factors such as diet, lifestyle, emotional state, and environment.
In clinical practice, we are privileged to have the ability to hear what our patients are presenting with, or their story. We have the capacity to order testing to look at their phenotypical expression. The phenotypical expression describes what each gene is telling the body to say. In other words, the “stories” told. This allows not only to offer better treatment of existing concerns but also to tailor the prevention of future disease.
DNA: A Patient Study
I saw this first-hand through the story of one of my patients, JP. When we met, JP told me “I would love to find relief from the gut pain I feel daily… I can’t remember the last day I had without some bowel pain or issue like gas and bloating.” Alongside her severe digestive symptoms, JP expressed significant anxiety, fatigue toward the end of the day, fertility concerns, and cravings for sweets.
JP was a bright, young individual experiencing undue suffering every day. The issues left unresolved by conventional care were not only causing daily pain and discomfort but put JP at risk for developing serious illness in the future.
To get to the root-cause of JP’s suffering, I ran the following tests:
Enterolab
This uncovered hidden celiac disease, as well as casein (dairy) intolerance.
MRT LEAP
This showed 35 “reds” and “yellows” (food sensitivities), suggesting severe intestinal permeability.
GI Stool Effects
Showing SIBO (Small Intestinal Bacterial Overgrowth) and various medication intolerances.
Neurotransmitter Testing
Showing imbalances that could aggravate and perpetuate her anxiety.
Heart Rate Variability
Showed a stressed system in need of rest and relaxation.
ION Panel
Her ION revealed numerous nutritional imbalances. These allowed for exploration into ‘nutrigenomics’, or how these nutrient deficiencies and imbalances affected JP’s gene expression and determined her health.
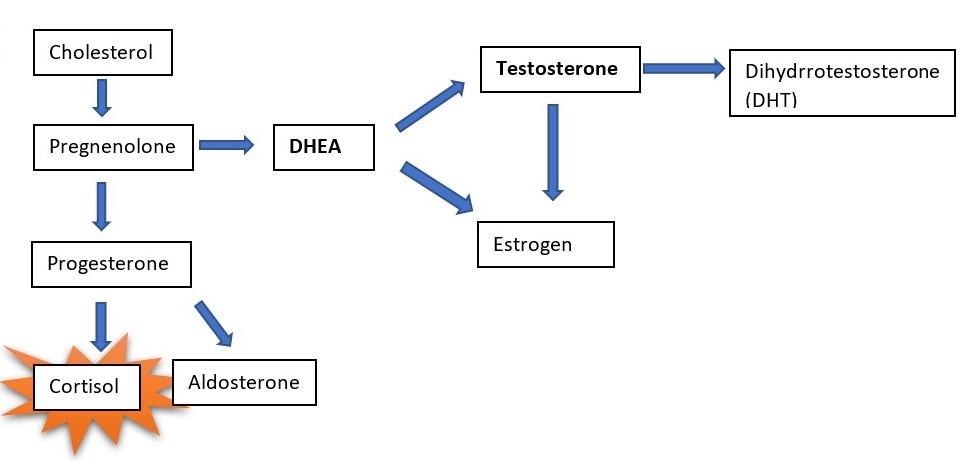
All of the above tests allowed for a greater understanding of the underlying imbalances that lead to JP’s debilitating symptoms. This allowed me to eliminate her lifelong digestive problems by cleaning up her gut, reducing her toxicity, balancing her hormones, and replenishing her nutrient depletions.
Her anxiety, however, began to worsen once her digestion improved. It was only in looking at her genome that I was able to finesse her diet and supplement program to heal her fully.
23andMe DNA Gene Test
Prior to the deciphering of the human genome, humans believed that once we knew the code of life in our DNA, we would answer all the questions related to the origin of disease. In reality, we learned that rather than disease being locked-in as hardwired “stories” in our genome, these characteristics included in our genes are dynamic. Each gene is in a constant dance with our environment, lifestyle, diet, stress level, and physical activity (or lack thereof).
In running the 23andMe DNA gene test, we uncovered genetic inefficiencies in methylation, neurotransmitter sensitivity (mood management), and nutrient usage (explaining the nutritional imbalances). We received information so we could optimize her diet and realized how to reduce her risk for the mood disorders most of her close family suffered from. The ability to improve her addictive behavior around sweets, and greatly reduce the risk of her developing the chronic illnesses she was particularly susceptible to getting.
Thanks to genomic testing, I was able to see where JP’s gene expression was hindering her healing journey. With that knowledge, we were able to build bridges where there were once roadblocks, and JP left my office with the gifts of vitality and robust health.
The Genomic Revolution and Paradigm Shift in Healthcare
“Our health and disease patterns are not hardwired by our genes, but are rather a consequence of the interaction of our genetic uniqueness with environmental factors.”
Jeffery Bland, PhD
Jeff Bland called this genomic revolution a paradigm shift in our model of healthcare from a deterministic, disease-centric model to a wellness-centric model. We assumed dominant and recessive traits were locked into our genes with no ability to change them. The assumption said that medicine existed to put a band-aid on symptoms and disease which we could not prevent or heal. Luckily, our new wellness-centric model asks not only “How do you get sick?”, but “How can you be well?”.
We are on a gigantic wave of a medical revolution, and genomics is at the heart of that wave. Let’s paddle out together and see where the riptides might be.
About the author:
Dr. Murfin is wholeheartedly focused on her life’s mission to help people heal and achieve extraordinary outcomes. She believes that health is more than merely the absence of disease. It is a total state of physical, mental, emotional, spiritual, and social wellbeing through the creation of a whole and meaningful life. Dr. Murfin leaves no stone unturned to determine the root cause of illness or imbalance.