Most of us are not living in line with our natural biological rhythms. This is causing imbalances in our hormone levels. Hormone imbalances often affect our brain’s ability to function efficiently and can cause obesity, dementia, mental health disorders, and many other serious health issues. Keeping our sex hormones in check is critical to our overall well-being.
Signs your sex hormones are out of balance:
- Depression and anxiety
- Exhaustion
- Trouble concentrating
- Sleep issues
- Being overweight or having excessive belly fat
- Sugar and salt cravings
- Menstrual pain and premenstrual syndrome (PMS)
- Challenging menopause or andropause symptoms
- Mood and energy swings
- Low sex drive
- Needing caffeine or alcohol to function
At Linden & Arc Vitality Institute, we are experts at addressing and treating hormone imbalances. Our goal is to support your body by restoring and improving your health and well-being.
What Are Hormones?
Hormones are produced and managed by our endocrine glands. They are chemical messengers in our bodies that are secreted directly into our bloodstream. They move to all parts of the body to help control how cells and organs work. Hormones help us manage our moods, sleep, growth, thyroid, sexual behaviours, stress responses, and blood sugar levels.
Because the control centers of your endocrine glands are in your brain, even a slight imbalance of your hormones can alter your brain’s capacity to learn and function effectively. Meaning your hormones can affect all aspects of your life!
Your sex hormones affect your sexual development, reproduction, and many other aspects of your life. These hormones include testosterone, estrogen, pregnenolone, progesterone, and DHEA (dehydroepiandrosterone).
Testosterone
Testosterone is a brain-boosting sex hormone responsible for building muscle mass and improving all genders’ mood, memory, motivation, and cognitive function.
Testosterone levels tend to drop with age due to weight gain, little exercise, chronic stress, and high sugar diets. Birth control, surgical menopause (surgical removal of the ovaries), and medications can also lower testosterone levels.
Signs of low testosterone:
- Low sex drive
- Erectile dysfunction
- Less sensitive clitoris
- Decreased sense of well-being
- Depression
- Decreased concentration and memory
- Fatigue
- Mood changes
- Decreased muscle strength
- Increased cellulite or varicose veins
- Joint pain
- Hair loss
Those born males often experience symptoms of andropause as they reach their 40s. Andropause happens as testosterone levels decline with age. Symptoms include depression, fatigue, loss of mental clarity, and loss of sex drive and function. These symptoms are avoidable and are caused by hormone imbalance.
Regular exercise and strength training, ensuring you are eating enough protein, fat, and whole carbohydrates, getting plenty of sleep, and reducing stress are great ways to help raise your testosterone levels.
Many excellent delivery systems are available to easily keep your testosterone levels optimized and balanced, including Bio-Te pellets, creams, lozenges (troches), and injectables.
Estrogen
Everyone’s body makes and needs estrogen! Estrogen promotes the production of serotonin, making it one of nature’s natural antidepressants! Like all hormones having imbalanced estrogen levels can send your body into crisis.
In the brain, estrogen has been shown to reduce the risks of dementia, while too much can cause breast, uterine, and cervical cancer, as well as breast growth in men.
Adrenal glands, ovaries, and fat tissues produce estrogen. All genders have this hormone, but those born female create more of it. As we age, our adrenal glands start to make most of our sex hormones. Bad habits such as smoking, alcohol consumption, high sugar and refined carbohydrate diets, and chronic stress deplete our adrenal glands.
Symptoms of premenstrual syndrome, brain fog, memory loss, mood swings, hot flashes, vaginal dryness, and sleepless nights due to menopause are not inevitable. They are treatable symptoms that are caused by hormonal imbalances.
Signs of estrogen imbalance:
- Fatigue
- Weight loss or gain
- Irregular or no periods
- Mood swings
- PMS
- Hot flashes
- Sore breasts
- Headaches and migraines
- Decreased sex drive
- Depression and anxiety
- Infertility
- Increased hunger and thirst
- Sensitivity to hot or cold
- Bowel movement changes
- Frequent urination
- Stretch marks
- Blurred vision
Maintaining a moderate weight, regular exercise, reducing stress, consuming proper nutrients, and taking care of your gut health are great ways to help balance your estrogen levels.
Estrogen Detox
Your body naturally detoxes estrogen using a 3-part process.
Phase 1: Estrogen is turned into three types of metabolites including 2-OH, 4-OH, and 16-OH.
Phase 2: A process called methylation neutralizes 2-OH and 4-OH. This makes the metabolites water soluble so that they can be safely excreted from the body.
Phase 3: Excretion – If your gut bacteria is agitated and you produce too many enzymes, this phase will not work, and recirculation will occur. This leads to inflammation and estrogen dominance.
How to promote estrogen detox:
- Try a whole food plant-based diet (avoid soy). Plant foods support hormone balance and microbiome.
- Reduce plastic use. Plastic contains synthetic estrogens, even when it is BPA-free plastic.
- Reduce stress.
- Take care of your gut and ensure you have regular bowel movements.
- Exercise regularly.
- Limit alcohol intake.
- Ensure you are getting proper sleep.
Pregnenolone
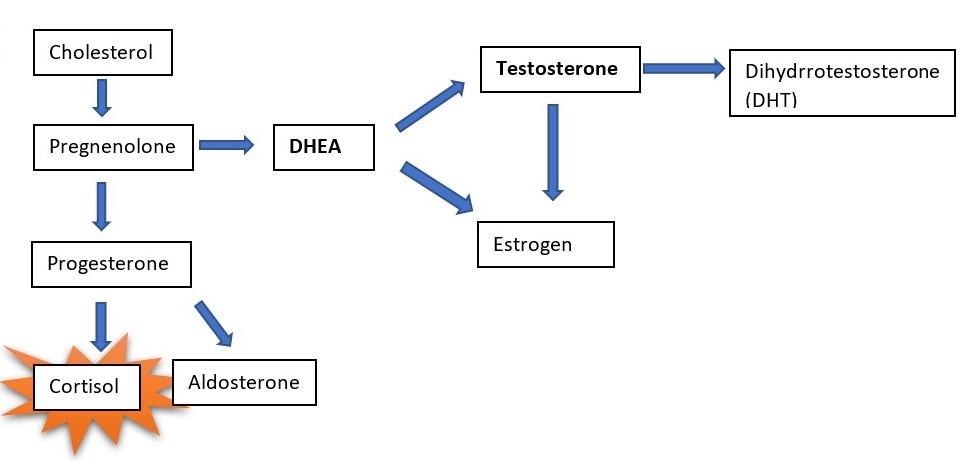
Some call this the “mother of hormones” because it is the steroid hormone used as a precursor to making all the other steroid hormones in a process called steroidogenesis. Pregnenolone is made from cholesterol in the adrenal glands, brain, ovaries in females, and testes in males. The synthesis of each class of hormones is dependent on various factors, including the location of where it is being made, the enzymes involved, and the other hormones present.
There are five classes of steroid hormones synthesized from pregnenolone, including:
- Androgens (Ex. testosterone, dihydrotestosterone (DHT))
- Estrogens (Ex. estradiol)
- Glucocorticoids (Ex. cortisol, corticosterone)
- Mineralocorticoids (Ex. aldosterone)
- Progestins (Ex. progesterone)
Pregnenolone also has other actions in the body. It has anti-inflammatory effects and is immune supporting. When pregnenolone is made in the nervous system, it is called a neurosteroid. Neurosteroids influence gene transcription and modulate neurotransmission. This results in various effects on brain function and supports neuroprotection. If your pregnenolone production declines, the hormonal imbalance often results in struggles in your day-to-day life.
Low pregnenolone can show as:
- Poor memory & trouble concentrating
- Fatigue
- Decreased sex drive
- Dry skin
- Muscle & joint stiffness
Progesterone
Progesterone is what we like to call a magical unicorn hormone! It helps soothe and calm our nervous system and supports our capacity to manage stress.
Progesterone is a sex hormone produced in both men and women and plays a significant role in testosterone production. It is produced in a woman’s second half of her menstrual cycle after ovulation. It plays a role in maintaining blood flow to the uterine lining, regular menstrual cycles, pregnancy, and normalizes periods (not too light and not too heavy).
Progesterone levels can drop due to nutrient depletion, stress, consuming too many saturated fats and refined sugars, certain medications (especially antidepressants), overexercising, and decreased thyroid functioning. When progesterone drops in relation to estrogen – either relatively or absolutely – PMS occurs.
Low progesterone can show up as:
- Anxiety, nervousness, irritability, moodiness, and lethargic depression
- Insomnia – unable to get into that deep, restorative sleep and therefore restless sleeps and waking up tired
- Decreased libido – this symptom is also shared with low testosterone and DHEA
- Headaches (especially around your period)
- Weight gain
- Lighter or skipped periods
- Spotting before your period
- PMS: acne, bloating, breast tenderness, water retention
- Estrogen dominance signs – heavy periods, painful periods, fibroids, endometriosis, cysts, and fibrocystic breasts.
If you identify with any of the listed symptoms above, know that there are many ways we can naturally support your sex hormones balance. Here are a few lifestyle tips to get you started:
- Get better sleep – prioritize your sleep and make it your non-negotiable! No matter who you are, 8 hours is still the recommended minimum amount of sleep per night.
- Consume good quality, healthy fats – our hormones use cholesterol as their backbones!
- Try castor oil packs placed on the body over the liver (see link). The liver detoxifies all our hormones, and castor oil can help clear excess estrogen from the body that can contribute to progesterone deficiency. At Linden & Arc, we recommend the Queen of Thrones Castrol Oil Pack.
DHEA
Dehydroepiandrosterone (DHEA) is another one of your sex hormones. It is made by your adrenal glands, with a small amount also being made in your brain and skin. DHEA makes your estrogen and testosterone and has been shown to have protective effects against cancer, diabetes, obesity, high cholesterol, heart disease, and autoimmune disease.
DHEA production declines with age, starting in your late twenties, and by the age of seventy, your body only makes one-fourth of the amount it made earlier. All too often, the focus is on estrogen, progesterone & testosterone as a first step. However, the doctors at Linden & Arc start balancing the hormones of Metabolic Triad 1: adrenal, thyroid, pancreas as an integral first step to wellness and reclaiming your energy.
DHEA helps to:
- Decrease allergic reactions
- Decrease cholesterol
- Deal with stress
- Increase brain function
- Increase sense of well-being
- Prevent blood clots
- Promote weight loss
- Reduce insulin resistance
- Support your immune system
- Reduce blood sugar spikes
DHEA deficiencies often occur due to aging, nicotine, menopause, or stress.
Symptoms of DHEA deficiencies include:
- Decreased energy
- Decreased muscle strength
- Difficulties with stress
- Irritability
- Joint soreness
- Weight gain
If your body has low DHEA levels, DHEA hormone replacement may be an excellent option for you.
How Linden & Arc Vitality Institute Can Help You Diagnose and Treat Hormone Imbalances
If you are experiencing symptoms of sex hormone imbalance, Linden & Arc Vitality Institute will take a thorough history of your hormone function. Our doctors will access your hormones using blood, urine, and saliva tests.
We use some of the most advanced tests to access hormone levels accurately. Saliva testing measures cortisol, estrogens, progesterone, and androgens levels. Our blood tests allow us to measure insulin, thyroid, and other hormone levels accurately. Urine is used to evaluate estrogen metabolism ratios. Estrogen metabolism ratios are how we gauge the pathways through which estrogen and sex steroids are detoxified from your body. We can also measure cortisol, progesterone, testosterone, and other hormone levels with urine samples.
We recommend a hormone test for everyone around ages 35-40, so we can measure your baseline labs and ensure you continue to have a good quality of life.
Once we have defined your hormone imbalance and addressed the cause, we will help your body restore and replenish balance using bio-identical hormones. Bio-identical hormone therapy (BHRT or natural hormone therapy) uses hormones that are identical to those your body produces on a molecular level.
Benefits of Bio-Identical Hormone Therapy:
- Mental clarity
- Increased energy
- Increased sex drive
- Increased ability to lose fat and gain muscle
- Decreased anxiety and depression symptoms
- Improved sleep quality
- Improved well-being
- Improved skin and hair health
At Linden & Arc Vitality Institute, we aim to break the cycle of unnecessary suffering with proactive treatments that will improve your quality of life. Our Functional Medicine practice seeks to uncover and treat the root cause of your illness, healing you as a complete being, not just a collection of symptoms.
If you are experiencing symptoms of hormone imbalance, click HERE, call 1-587-390-0180, or email [email protected], and we will guide you through how Linden & Arc Vitality Institute can help you.
Author:
Dr. Ayla Lester, ND