Cold Submersion Therapy or Cold Water Immersion (CWI) is an ancient hydrotherapy treatment. It relieves many ailments and chronic symptoms. People suffering from immune system or mood disorders, have trouble sleeping or have increased stress levels can benefit from this type of therapy. This form of hydrotherapy is similar to aquatic therapy, pool therapy, or balneotherapy. The use of water in various forms and at various temperatures produces amazing effects on the human body.
In Activating the Vagus Nerve: Part 1 – Breathe!, we explored the positive effects that breathwork has on our Vagus Nerve. How we breath affects our autonomic nervous system – which has two branches, sympathetic (fight or flight) and parasympathetic (rest and digest). You can think of the sympathetic as the gas pedal on your system and the parasympathetic as the brakes. Let’s now dive deeper into how we can manipulate the nervous system and make it stronger by introducing cold water immersion (CWI) therapy while we are breathing.
“Cold water? What the … ?!” You might exclaim, especially if you are living in a cold climate like Calgary, Alberta.
Taking actionable steps like CWI therapy can help reduce stress levels. CWI is an ancient therapy used to relieve many ailments. People suffering from immune system or mood disorders, having trouble sleeping, or increasing stress levels can benefit from this type of therapy. Here we outline some reasons why CWI is so good for you. It enhances your immune function, boosts your metabolism, elevates your mood, and builds endurance.
Reasons to try CWI
Enhance Your Immune Function
Cold Submersion Therapy stimulates immune function. It does this by stimulating the white blood cells. They then provoke the white blood cells to attack and destroy toxic substances in the lymph fluid. The cold water positively affects the lymphatic system, affecting the immune system by flushing waste and toxins.
Boost Your Metabolism
Cold Submersion Therapy helps to boost your metabolism, which can assist with weight loss efforts. This is not to be substituted for a healthy diet and regular exercise. This practice makes your body work harder to keep you warm, which inadvertently burns calories. It also affects the type of fat the body produces. According to a study done in 2009, brown fat (BAT), or good fat, mobilizes when your body becomes exposed to frigid temperatures. It works to keep us warm, thus eliminating white fat, which is the fat that sits around your thighs and waist.
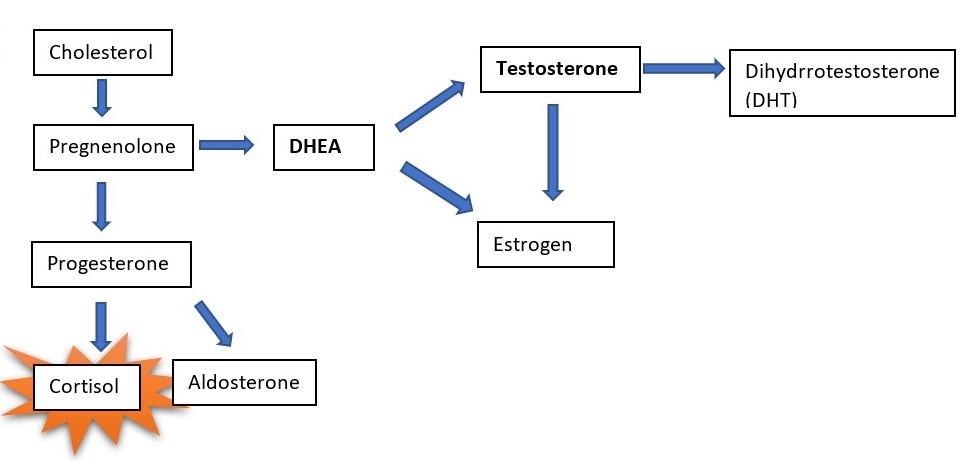
Improve Sleep, Reduce Stress, & Elevate Mood
When we sleep, our bodies heal, so it is vital to get adequate restful sleep. CWI reduces muscle soreness and pain, which allows you to sleep more soundly. Quality sleep will, therefore, reduce stress levels and elevate your overall mood.
Build Endurance & Resilience
The thought of submerging your body in cold water makes most people cringe, but it is suitable for your body and your mind! It is a good practice in mental strength, endurance, and resilience which requires you to break out of your comfort zone. I learned that cold never stops being hard. It never gets easier, but your mind has become more resilient and robust. Immersing your entire body in ice water trains your brain to control your responses to stress, pain, and anxiety, instead of allowing your emotions to overwhelm you. Try reframing your thoughts with mindful breath and action by breathing through sensations and feelings that arise. CWI will allow your body and mind to work through a state of stress and enter a state of calm. Don’t forget to breathe, as this is so crucial. When our breathing is full and deep, the diaphragm moves through its entire range downward to massage the internal organs and tissues below it and then moves upward to massage the heart. Training the body to control the breath and negative mind chatter can be a total game-changer for anxiety and depression.
If cold water immersion still isn’t seeming like your thing, try ending your showers with cooler water temperatures. You can start slowly and build up to longer stints of colder temperatures. Breath through the discomfort and find a motto to help build your resilience, such as “I am more than my thoughts,” or “I choose to step into mindful, peaceful action”, and “I am stepping away from fear.”
The cold never stops being cold but taking actionable steps that you can implement into your daily/weekly routine will guide you towards taking back control over your health by increasing resilience in your mind and body. How powerful is that! Challenge yourself today by trying the Wim Hoff method of Cold Submersion Therapy along with deep diaphragmatic breathing for your overall health. Take the plunge!
Author:
Darla Montgomery