Most often, inflammation is rooted in the gut and caused by food sensitivities. These days we encounter an epidemic of chronic health issues resulting from inflammation. By understanding the gut in more detail, we have the capacity to decrease inflammation without the use of medications that have long lists of side effects and don’t solve the underlying issue.
The important thing to realize about inflammation is that it can appear in any part of the body, including hormone systems, the brain, and the cardiovascular system. The evidence for this is unquestionable. This being said, it is very important to identify foods that may be stimulating our immune system and having detrimental downstream health effects.
Testing for food sensitivities has its controversies, but it can be a very useful starting point. IBS and Crohn’s disease respond best to IgG testing but are clinically applicable in many other illnesses. The tests reveal gut complaints, chronic fatigue, depression and anxiety, and autoimmune issues, to name a few.
Limitations of food sensitivity testing:
1. They test only limited immune reactions and do not show non-immune food reactions
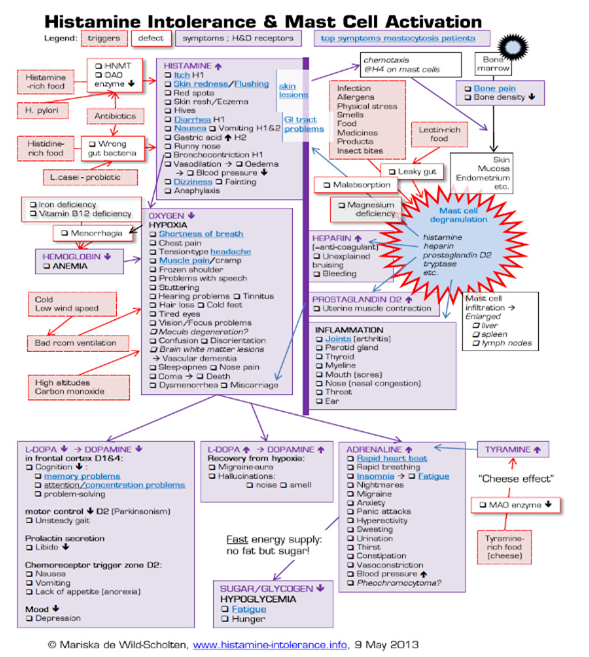
Food sensitivity testing is not perfect, as it is only testing a very select part of the immune system. Parts of the immune system most often tested are IgE (true allergy), IgA (mucosal immune system), and IgG (delayed food sensitivities). A negative test does not exclude a reaction by the innate immune system, or a non-immune reaction (like lactose intolerance, FODMAP intolerance, or histamine intolerance).
2. Laboratory standards differ
The accuracy of testing can vary from lab to lab, depending on which controls and which antigens they use. For example, an organic apple may have different reactivity to one that is not organic. Heat and processing or roasting may make an antigen more or less antigenic. Whether the lab uses monoclonal antibodies (from one source) vs polyclonal antibodies (from many sources), can also affect the reactivity of the test.
3. Individual and confounding factors
False positives may result from smoking, alcohol consumption, periodontal disease and other factors. False negatives may result from immunoglobulin deficiencies. Lab tests may not pick up individual differences in immunoglobulins which could also skew results.
Testing often shows reaction to antigens which should be ‘healthy’ foods. This situation is often caused by increased intestinal permeability. Something like gluten may trigger leaky gut, allowing bystanders to leak through the gut layer and stimulate an immune reaction. Gut repair is essential in resolving this.
With all these confounding factors, how do you figure out what you are reacting to?
The gold standard of figuring of food sensitivities is with an elimination diet. This means taking out the common allergenic offending foods for a period of 3-4 weeks minimum and then slowly reintroducing them one by one. A positive test results when a reaction to the reintroduced food occurs.
In an ideal world, every patient with a chronic health condition should go through an elimination diet. Unfortunately, this does not always happen. In many cases, people do not believe that their health condition is related to food and so are not willing to change their way of eating.
The benefits of food sensitivity testing:
Enter the food sensitivity test. Though not all testing is perfect, this can be an extremely useful tool in figuring out major food triggers. Keeping the above limitations in mind, improvements in symptoms should occur with removal of the offending foods. The proof is in the pudding: people very often do get dramatically better when they remove the positive foods on the tests.
When they do not get better after a trial of elimination, a skilled health care professional will guide the patient to work through different steps based on their history, physical examination and testing, to figure out what is causing their symptoms.
Reasons people don’t get better:
- Gut healing not done alongside the removal of the problem foods. Much research around gluten removal with or without gut repair, has been done. A large percentage of patients do not improve symptomatically when the gut repair is not undertaken. This involves replacing pancreatic enzymes, gallbladder support, and stomach acid and healing the lining of the gut.
- The person is reacting to food in a different way. They may have histamine, salicylate, or oxalate intolerance or a lectin intolerance and respond to a grain and legume-free diet. They could also have fructose intolerance.
- They may have dysbiosis, or overgrowth of bacteria/ yeast or parasites (often interrelated with food sensitivities). Because of this they may have FODMAP intolerance (with SIBO) or may react to foods that trigger candida, like sugar.
- They have a misunderstanding about which foods contain the antigens they are reacting to or are being inadvertently exposed to. A common example is gluten, found in many spices, teas, toothpaste, etc.
- Their symptoms may not be directly related to the gut and can be related to heavy metal toxicity, biotoxin illness (mold commonly causes gut issues) or autonomic imbalance.
- They had a false positive test.
The good news
The aim is not to be off the offending food forever – the aim is to figure out why someone is reacting in the first place. If you heal your gut and eliminate correctly, you should be able to eat most things again but some people may need to stay off certain foods lifelong. The most common of these are gluten, dairy, and eggs.
The bottom line is that food sensitivity testing is far from perfect, but it is very often a starting point to guide a patient in the right direction and motivate lifestyle changes. The important take home is to ask why the food reactions are happening in the first place. On many occasions, people become frustrated because they follow the elimination of the foods found on their tests and they don’t feel better. It is essential to have an experienced health care provider interpret your food sensitivity test in the context of what your issues are so that you can be guided in the right direction and achieve the best results.
References
Bentz, S., Hausmann, M., Piberger, H., et al., (2010). Clinical relevance of IgG antibodies against food antigens in Crohn’s disease: A double-blind cross-over diet intervention study. Karger – Digestion 81(4), 252-264. https://doi.org/10.1159/000264649
Drisko, J., Bischoff, B., Hall, M., & McCallum, R. (2005). Treating irritable bowel syndrome with a food elimination diet followed by food challenge and probiotics. Journal of the American College of Nutrition 25(6), 514-522. https://doi.org/10.1080/07315724.2006.10719567
Guo, H., Jiang, T., Wang, J., et al., (2012). The value of eliminating foods according to food-specific immunoglobulin G antibodies in irritable bowel syndrome with diarrhoea. Journal of International Medical Research 40(1), 204-210. https://doi.org/10.1177/147323001204000121
Meletis, C.D., & Barker, J. Delayed-onset food allergies (2004). Alternative and Complementary Therapies 9(2), 61-65. https://doi.org/10.1089/107628003321536968
Uzunısmaıl, H., Cengız, M., Uzun, H., et al., (2012). The effects of provocation by foods with raised IgG antibodies and additives on the course of Crohn’s disease: A pilot study. Turkish Journal of Gastroenterology 23(1), 19-27. DOI: 10.4318/tjg.2012.0332
Zar, S., Mincher, L., Benson, M.J., & Kumar, D. (2005). Food-specific IgG4 antibody-guided exclusion diet improves symptoms and rectal compliance in irritable bowel syndrome. Scandinavian Journal of Gastroenterology 40(7), 800-807, https://doi.org/10.1080/00365520510015593
Author
Dr. Michelle van der Westhuizen, MD